A Heart Attack is an Accident Waiting to Happen: A Deep Dive into the Swiss Cheese Model of Disaster Prevention.
A Cardiologist Perspective:
Ever since 1996, following three years researching ‘coronary thrombosis’ for my MD thesis and then during the 25 years spent as an interventional cardiologist dealing with heart attacks, I’ve been curious about why some people who have a small amount of coronary artery plaque and few risk factors for heart disease can have an unexpected and fatal heart attack, while others with more coronary plaque, many risk factors, and little treatment, can live for 30 more years without any heart attack or symptoms, even though they had their first one when they were young. The only reasonable explanation I can think of is that with heart disease, as in life in general, luck or chance also plays a role.
When we think about accidents, we often view them as isolated incidents, anomalies in an otherwise predictable flow of events. But accidents, like a plane crash or indeed a heart attack, as explained below, can be the culmination of a series of underlying causes. Rather than being considered as a single chance event, there may be a chain of causative factors, that, when aligned perfectly, pave the way to catastrophe. Understanding this perspective can shed light on how to prevent accidents in a myriad of scenarios. In this regard, one model stands out in illustrating this phenomenon – the Swiss Cheese Model of system accidents [1].
The Swiss cheese model can assist to explain complex systems and how multiple layers of defence can fail, leading to an adverse event. In the context of heart disease, it can also help illustrate how various factors can interact and explain why for example, effective prevention of heart attack involves more than just the taking a statin.
Unpacking the Swiss Cheese Model
Imagine a stack of spinning disks, each a piece of Swiss cheese with holes of different sizes “.. slices of Swiss cheese, having many holes—though unlike in the cheese, these holes are continually opening, shutting, and shifting their location. The presence of holes in any one “slice” does not normally cause a bad outcome. Usually, this can happen only when the holes in many layers momentarily line up to permit a trajectory of accident opportunity—bringing hazards into damaging contact with victims.” [1]
The analogy goes that an accident only occurs when all the holes, representing different failures in the components of the whole system, align. A hole in any one layer does not create the event. This is a chance event, more likely the larger the holes, and less probable when the holes are reduced in size. The objective, then, is to decrease the risk of accidents by reducing the size of these holes, working on multiple layers rather than just one. It’s a model that helps us understand the probability of mishaps, and to devise preventive measures by focusing on every possible risk layer.
If we use the swiss cheese model to understand the apparently random nature of an unheralded heart attack, which can sometimes be associated with sudden cardiac death, we must first understand that, unlike in aviation industry where design, funding, culture and training represent ‘risk layers’, in heart disease the ‘layers of cheese’ are biological and physical processes that affect the coronary arteries, which are just 2-3 mm in diameter and supply the heart with oxygen and energy. A heart attack happens by chance as multiple layers interact and the ‘holes’ in each of at least 4 layers depicted in the diagram below, by chance line up. It must be understood that even large holes in any one layer on its own is not sufficient to cause a heart attack- which explains why some fortunate people with high cholesterol levels in their blood and large amounts coronary artery cholesterol deposits can survive for many years without developing symptoms, yet a unlucky person with a much smaller amount of the same process affecting their coronary arteries can suffer a fatal heart attack at a young age- it is the interaction between all the layers and the play of chance that explains the different clinical presentations.
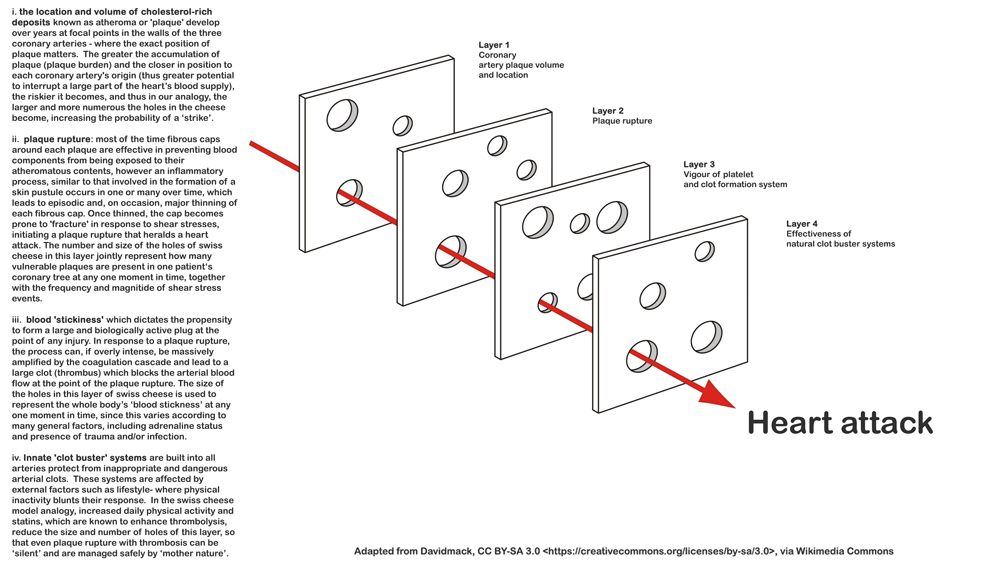
Fig 1. Four identifiable ‘risk’ layers contribute to a heart attack in an individual patient, where the risk of a heart attack can be linked to the number and size of the holes in each layer. Whereas the holes in the first layer can change over many years those in the latter layers vary day by day and even hour by hour. The four layers are spinning and the holes in three of the four distinct layers constantly vary in size as they open and shut thus only align infrequently by chance, explaining the random timing of a heart attack as well as why one patient, even left untreated can have their second event decades after their first.
The Story of Cholesterol
To illustrate this model effectively, let’s look at patients with high cholesterol levels, a condition that increases the risk of heart disease. Just like a stack of Swiss cheese, coronary artery disease (CAD) also builds up layer by layer, beginning as early as in our 20s with the development of fatty streaks in the arteries.
Over many years, bad cholesterol (LDL cholesterol) passes through the arterial layers, causing an inflammatory response. Our body’s white cells try to capture and transport these inflammatory chemicals out of the wall, but not all can be removed. This residual contributes to the evolution of fatty streaks into liquid plaque that accumulates inside and outside the artery wall. Calcification in the coronary plaque signals the advanced stages of the disease. So, the first layer in the Swiss cheese model of heart attacks is the development of plaque in the artery walls, the extent and volume of which affects future risk and without which a myocardial infarction or ‘heart attack’ is unlikely to happen.
The existence of this first layer is why doctors believe that a sensitive technique that measures both coronary plaque and inflammation may be such a game changing technology that we can start to use to predict personal risk of future symptomatic CAD in anyone over the age of 40 [2,3].
The Thin Line between Stability and Disaster
When atherosclerosis progresses and plaque builds up within the walls of arteries, the affected area becomes susceptible to a phenomenon called “plaque vulnerability.” Plaque vulnerability refers to a state where the plaque composition undergoes changes that make it more prone to rupture. These changes can include a temporary thinning of the fibrous cap that covers the plaque. In time, assuming no major rupture occurs, natural healing strengthens the thinned area and the period of increased vulnerability to rupture (and heart attack) is passed. The fibrous cap is thus a protective layer that encapsulates the plaque, keeping its lipid-rich core contained and preventing its exposure to the bloodstream. At times when the fibrous cap can become thinner and weaker, it is susceptible to mechanical forces.
Now, let’s consider the sudden peaking of blood pressure, which can be triggered by various factors such as stress, physical exertion, or an adrenaline surge. When blood pressure rapidly increases, the force exerted by the blood flow against the arterial walls also increases. This sudden increase in blood pressure can generate a significant shear stress on the plaque. Shear stress is a mechanical force that acts parallel to the surface of the plaque. The fibrous cap, especially when already weakened due to plaque vulnerability, may not be able to withstand the sudden shear forces applied to it. As a result, the fibrous cap may rupture or tear, exposing the lipid-rich core of the plaque to the bloodstream.
The second layer of the model therefore relates to the variation in risk which occurs as the cap that separates the plaque from the circulating blood thins. If the biological process that thins or softens this fibrous cap by chance coincides in time with a shear stress event (such as unaccustomed burst of exercise or activity that causes the blood pressure to peak) a plaque rupture follows. Like a pustule, the fibrous caps of a vulnerable plaque can, in any case, thin over time due to an active inflammatory process, thus a rupture can happen unprovoked, but it is most likely to occur during high shear stress. If good fortune intervenes, no rupture occurs, and healing ensues. If not, the plaque’s contents are exposed to the blood, leading to a thrombotic reaction. Hence, the lipid pool and the development of a vulnerable plaque represent the second layer in the cheese model. This concept helps explain cardiac events linked to shovelling snow, the first mow of the season and pushing ones’ car that has got stuck in the mud or snow – all events that produce a peak in shear force on any vulnerable plaques.
Understanding these mechanisms can help in developing strategies to manage and prevent cardiovascular events associated with atherosclerosis and plaque rupture.
Thrombosis and Platelets: The Silent Guardians
When the core of the plaque is exposed following a plaque rupture, platelets and other components of the blood can come into direct contact with the lipid-rich material. This triggers a series of events that can lead to the formation of a blood clot or thrombus at the site of the ruptured plaque. The third layer addresses the thrombotic reaction to a plaque rupture.
It’s known from autopsies of road traffic accident victims that multiple plaque ruptures can occur silently, without any symptoms, with circulating platelets acting as first responders to these events. When behaving optimally, platelets form an organised plug that seals off the area, protecting against the exposure of larger thrombotic proteins that form the coagulation cascade.
However, the vigorousity of this platelet-dependent step is known to vary significantly. During periods of generalised high platelet activation, such as when the body is dealing with an unrelated infection or stress far away from the heart, even a minor coronary artery plaque ruptures could trigger a more aggressive platelet response which can trigger amplification through recruitment of coagulation proteins and a chain reaction follows that causes the vessel to occlude with a red clot.
This variability in platelet activation and coagulability forms another layer in our model, explaining why not all plaque ruptures lead to cardiac symptoms and why antiplatelet drugs like aspirin and clopidogrel have proven efficacy in preventing acute coronary thrombotic events- in effect, antiplatelet drugs lower the risk of a vigorous platelet recruiting other blood proteins that leads to a cascade and formation of a clot that then blogs the artery. By taking even a 1/4 of a tablet of Aspirin, we affect this important layer in the process, which is what such drugs have proven so effective in helping to prevent heart attacks in those patients who are at risk.
Body’s Fibrinolytic Defence: Our Natural Clot Busters
The fourth layer concerns how the body deals with arterial thrombosis. Our arteries host a pathway of clot-busting proteins – the fibrinolytic pathway. These proteins are always on standby, ready to deal with a potential thrombus that could have life-ending consequences by causing end organ damage. This system is finely balanced to prevent arterial thrombosis during periods of activation such as exercise (as part of the natural flight or fight response), while simultaneously being ready to prevent bleed outs in case of injury.
External factors such as statin therapy and regular exercise are known to improve an individual’s ability to deal with arterial thrombosis, whereas a sedentary lifestyle and diabetes predisposes to arterial thrombosis linked to heart attacks. The protective effect of exercise, especially by effects on the fibrinolytic pathway, is crucial in defending against dangerous arterial thrombosis. An effective ‘clot buster system’, represented by smaller holes in the last spinning plate in our model, can thus prevent a full ‘strike’ or heart attack, as natural and effective lysis of an arterial clot that has transiently blocked an artery can occur naturally, without a person even being aware that a life threatening incident has taken place.
Cardiac arrest
Sudden occlusion of a major coronary artery is known to be the most frequent cause of sudden death. The heart muscle develops unstable electrical activity in response to an interrupted blood supply yet there is considerable variation in this response- in effect a 5th layer of swiss cheese that determines each individuals response and risk of sudden death. This topic is expanded a separate blog “sudden death: the 50 year wave” to be released in Sept 2023.
Preventive Measures
Understanding the Swiss Cheese Model in the context of heart attacks allows us to consider each layer for the most substantial protective effect. Just as improving aviation safety requires a multi-faceted approach rather than focusing on a single issue, preventing a fatal heart attack should not merely be about obsessing over cholesterol-lowering statins. It should also involve inhibiting platelets, encouraging exercise, and in high-risk patients, considering beta-blockers.
In summary, the Swiss Cheese Model provides a clear perspective on how a multitude of factors, when lined up, can lead to a catastrophic event such as a plane crash or a heart attack. Each hole, or layer, represents a potential risk, and it is our collective responsibility to identify and reduce these risks. Through education, intervention, and awareness, we can work towards preventing these tragedies from happening.
Bibliography
1/ Reason J. Human error: models and management. BMJ. 2000;320:768–70. doi: 10.1136/bmj.320.7237.768. [PubMed]
2/ Subclinical Coronary Atherosclerosis and Risk for Myocardial Infarction in a Danish Cohort https://www.acpjournals.org/doi/10.7326/M22-3027
3/ Cardiovascular computed tomography imaging for coronary artery disease risk: plaque, flow and fat: Keith M Channon, David E Newby, Edward D Nicol, John Deanfield http://dx.doi.org/10.1136/heartjnl-2021-320265
4/ Does Exercise Influence the Susceptibility to Arterial Thrombosis? An Integrative Perspective https://www.frontiersin.org/articles/10.3389/fphys.2021.636027/full
5/ The Acute and Chronic Effects of Resistance and Aerobic Exercise in Hemostatic Balance: A Brief Review https://www.mdpi.com/2075-4663/11/4/74
